This article is reposted from the old Wordpress incarnation of Not Exactly Rocket Science. The blog is on holiday until the start of October, when I'll return with fresh material.
Many patients would like their doctors to be more sensitive to their needs. That may be a reasonable request but at a neurological level, we should be glad of a certain amount of detachment.
 Humans are programmed, quite literally, to feel each others' pain. The neural circuit in our brains that registers pain also fires when we see someone else getting hurt; it's why we automatically wince.
Humans are programmed, quite literally, to feel each others' pain. The neural circuit in our brains that registers pain also fires when we see someone else getting hurt; it's why we automatically wince.
This empathy makes evolutionary sense - it teaches us to avoid potential dangers that our peers have helpfully pointed out to us. But it can be liability for people like doctors, who see pain on a daily basis and are sometimes forced to inflict it in order to help their patients.
Clearly, not all doctors are wincing wrecks, so they must develop some means of keeping this automatic response at bay. That's exactly what Yawei Chang from Taipei City Hospital and Jean Decety from University of Chicago found when they compared the brains of 14 acupuncturists with at least 2 years of experience to control group of 14 people with none at all.
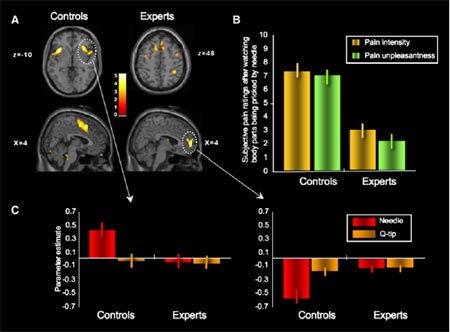
They scanned the participants' brains while they watched videos of people being pricked by needles in their mouths, hands and feet, or being prodded with harmless cotton swabs. Sure enough, the two groups showed very different patterns of brain activity when they watched the needle videos, but not the cotton swab ones.
The controls showed increased brain activity in areas involved in processing pain, including the anterior insula, anterior cingulated cortex, somatosensory cortex and the periaqueductal gray (or PAG). The PAG in particular is thought to act like a control centre for our panic response, mobilising our limbs into action when we sense danger.
In the brains of the more detached experts, these areas failed to light up. Instead, they showed increased activity in parts of the brain involved in higher functions like self-awareness and emotional regulation, including the parahippocampal gyrus, the middle frontal gyrus, the medial prefrontal cortex and the inferior parietal lobule (compare Figure C and D in the image below).
Even a needle in the mouth didn't provoke an empathic pain response in the experts, while these were most likely to activate the somatosensory cortex in the controls.
The participants' own answers to a questionnaire backed up the brain scans. When asked to rate the pain and unpleasantness shown in the needle videos, the controls gave an average score of 6.5 out of 10, while the acupuncturists felt the clips only warranted a 3 or 4 (figure B in image above).
Yawei and Decety ruled out the possibility that the doctors were just more emotionally numb than their controls, or more cavalier in the face of pain. In response to psychological questionnaires, the two groups showed no differences in their general levels of empathy or their sensitivity to pain.
Instead, the activation pattern in the experts' brains suggests that their higher brain functions block the activation of the pain circuit. The parahippocampal gyrus is partially responsible for retrieving memories - its activation allowed the experts to use their previous years of experience to influence their current reactions. The temporoparietal junction is important in maintaining a distinction between oneself and others, and its activation could allow them to emotionally detach from their patients.
With experience, the acupuncturists know that their actions are painful for their patients and have learned to repress their own automatic responses to the sight of pain. That may sound cold, but it's essential for operating a successful practice.
More on pain:
- Pain in the eye of the beholder
- Itch-specific neurons discovered in mice
- Thinking about money soothes sting of social rejection and physical pain
Reference: Cheng, Lin, Liu, Hay, Lim, Hung & Decety. 2007. Expertise modulates the perception of pain in others. Curr Biol 17: 1-6.
Image from Current Biology paper, Cell Press.




While I think this study is very interesting, a great follow-up would be to compare acupuncturists' responses to pain with those of more traditional medical doctors. Study after double-blind study has shown that acupuncture is pure placebo effect (google "Science Based Medicine" for more info) -- perhaps acupuncturists are aware on some level that their treatment isn't truly effective, and supress their response because of this? Just a thought. Thanks as always for a great article!
Gee. I'd cry, but my doctor wouldn't care.
Fortunately my shrink is a compassionate and insightful sort. Maybe I should have her handle my after-surgery care instead.
Why do you refer to acupuncturists as "doctors"? To do so lends credibility to these quacks.
I am a lowly phlebotomist, not an acupuncturist or a doctor, but I can absolutely vouch for the generalizability of this study to medical practitioners. I'm good enough at my job that most of the time I can keep it from hurting very much, but sometimes and with some procedures it's just not possible. In addition, in emergent situations pain management has to be way down on the list. A man had a heart attack in the ER last week (having walked in with chest pain), and he was zapped right there on the table, while still conscious. I've heard conscious cardioversion described as one of the most painful things a person can ever experience - but in this case, it saved the patient's life. If the medical staff had hesitated out of compassion for the patient's pain, his long term outcome would have been worse.
Acupuncturist = Physician???